Olympus Solutions for Lung Cancer Diagnosis and Staging
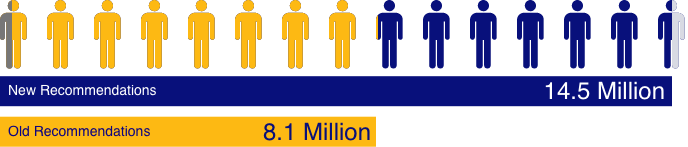
Lung cancer screening eligibility has been expanded. More patients than ever before will require accurate diagnosis and staging.3
Is your institution prepared?
Partner With Us
and staging and learn more about Olympus’ solutions.
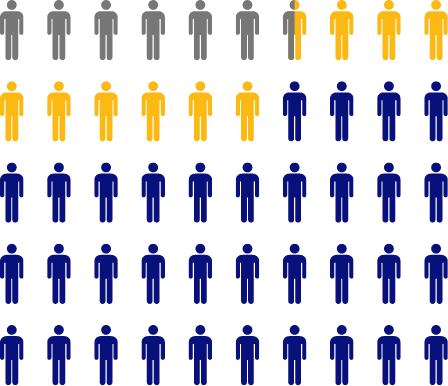
Clinical staging (radiographic imaging such as PET-CT) has been shown to be inaccurate 32% of the time when compared to pathologic staging (where tissue samples are obtained, such as EBUS-TBNA or mediastinoscopy). Inaccurate staging may lead to treatment decisions that are mismatched to disease progression.8**



EBUS-TBNA improves diagnostic accuracy in Lymph Node staging compared to PET-CT alone.10
Cancer, We’re Behind You All the Way.
Effective tools to drive the answers you need: Olympus can support your complete
diagnosis and staging solution.
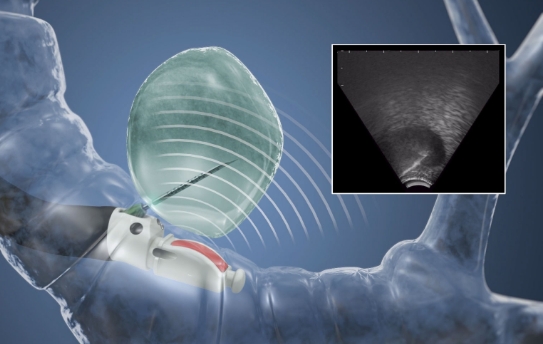
EBUS-TBNA is the guideline-recommended best first test for lung cancer diagnosis and staging.12 However, when a diagnosis with endobronchial ultrasound transbronchial needle aspiration (EBUS-TBNA) proves elusive, an effective approach for accessing and sampling the periphery is critical.
- EBUS-TBNA as the best first test over surgery for mediastinal staging.
- Radial EBUS for patients with a peripheral lesion and when tissue diagnosis is required due to uncertainty of diagnosis.
sampling portfolio.
in Real Time14
Real-time sampling and staging in one system is designed for efficiency and enhanced patient care.12


See a 360-degree image of the airway wall and surrounding structures external to the airway.14
Real-time ultrasound imaging supports direct visualization of the position of the lesion for sampling.14

Review data in support of Olympus Solutions for Lung Cancer Diagnosis and Staging.
Coming Soon

Gain access to our comprehensive training platform for ongoing learning opportunities and educational resources.
Dedicated Support Beyond Products

Count on reliable, end-to-end support — from the purchasing process to the procedure and reprocessing services — to maintain a relationship of lasting trust.
We’re Behind You All the Way.
Complete this form to get the latest information about Olympus solutions
for lung cancer diagnosis and staging.
*Initial recommendations issued in 2013 were based on NIST trial results and included patients 55 to 80 years of age with a 30-pack year history. United States Preventive Services Task Force (USPSTF) lung cancer screening guidelines have expanded after a closer look at the data, combined with evidence of the benefits of early detection and treatment.1-3
**Infographic shows the incorrect classification of patients who were falsely overstaged or understaged using PET-CT alone based on a prospective trial of 114 patients. PET-CT was compared to CT with similar findings of 27% falsely overstaged and 7% falsely understaged.6
1. Herth FJF, Ernst A, Eberhardt R, et al. Endobronchial ultrasound-guided transbronchial needle aspiration of lymph nodes in the radiologically normal mediastinum. Eur Respir J. 2006;28(5):910-914.
2. Fujino K, Ujiie H, Igai H, Kinoshita T, Lee C, Hindy S, Effat A, Yasufuku K. Human Ex Vivo Lung Evaluation of the Next Generation Convex Probe Endobronchial Ultrasound Bronchoscope. CHEST Journal 2017;152(4):A884.
3. U.S. Preventive Services Task Force. USPSTF Website. Accessed January 20, 2023. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
4. Li C, Wang H, Jiang Y, Fu W, Liu X, Zhong R, Cheng B, Zhu F, Xiang Y, He J, Liang W. Advances in lung cancer screening and early detection. Cancer Biol Med. 2022 May 11;19(5):591–608. doi: 10.20892/j.issn.2095-3941.2021.0690. Epub ahead of print. PMID: 35535966; PMCID: PMC9196057.
5. de Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med. 2020;382(6):503-513.
6. National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395-409.
7. Centers for Medicare & Medicaid Services. Decision Memo. CMS Website. Accessed January 20, 2023. https://www.cms.gov/medicare-coverage-database/view/ncacal-decision-memo.aspx?proposed=N&NCAId=274
8. Heineman DJ, Daniels JM, Schreurs WH. Clinical staging of NSCLC: current evidence and implications for adjuvant chemotherapy. Ther Adv Med Oncol. 2017;9(9):599-609.
9. Harders SW, Madsen HH, Hjorthaug K, et al. Mediastinal staging in Non-Small-Cell Lung Carcinoma: computed tomography versus F-18-fluorodeoxyglucose positron-emission tomography and computed tomography. Cancer Imaging. 2014 Jun 3;14(1):23.
10. Hwangbo B, Kim SK, Lee HS, Lee HS, Kim MS, Lee JM, Kim HY, Lee GK, Nam BH, Zo JI. Application of endobronchial ultrasound-guided transbronchial needle aspiration following integrated PET/CT in mediastinal staging of potentially operable non-small cell lung cancer. Chest. 2009 May;135(5):1280-1287. doi: 10.1378/chest.08-2019. Epub 2008 Dec 31. PMID: 19118267
11. Li S, Zheng Q, Ma Y, et al. Implications of false negative and false positive diagnosis in lymph node staging of NSCLC by means of ¹⁸F-FDG PET/CT. PLoS One. 2013;8(10):e78552. Published 2013 Oct 25.
12. Silvestri GA, Gonzalez AV, Jantz MA, et al. Methods for staging non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e211S-e250S
13. Herth FJ, Eberhardt R, Vilmann P, Krasnik M, Ernst A. Real-time endobronchial ultrasound guided transbronchial needle aspiration for sampling mediastinal lymph nodes. Thorax. 2006;61(9):795-798.
14. Data on File September 2019
Complications from extraluminal ultrasound-guided needle aspiration may include infection, bleeding, perforation and tumor seeding. Extraluminal fine needle aspiration of cystic lesions has a higher risk of complication from infection and bleeding.
Complications from bronchoscopy are rare and most often minor, but if they occur, may include breathing difficulty, vocal cord spasm, hoarseness, slight fever, vomiting, dizziness, bronchial spasm, infection, low blood oxygen, bleeding from biopsied site, or an allergic reaction to medications. Some patients may experience rare but more serious complications such as collapsed lung, respiratory failure, heart attack, and/or cardiac arrhythmia.


































